This past week I started a new rotation. This rotation will include the majority of my objectives from Medical Nutrition Therapy II and the Clinical Concentration. I will be here for about six weeks and am excited to take on a new challenge and get more experience in the clinical setting.
There are a variety of hospitals in the area and many dietitians that I will get to work with over the next few months so that I can experience the greatest diversity in patients and conditions. This first week I primarily spent my time with surgical and neuro patients on the floors and in the intensive care unit (ICU). Due to the severity of these patients’ conditions, many of these patients required tube feedings, which is also known as enteral nutrition – stay tuned for a post specifically about enteral nutrition! In the weeks to come I will have a chance to work with trauma, pediatrics, rehab, cardiac, behavioral medicine, weight loss, cystic fibrosis, diabetes, transplant, and even the wound clinic!
So before I get too far into this rotation I wanted to provide a little background so you can start to understand what exactly it is that a clinical dietitian does! A clinical registered dietitian (RD) will typically have following responsibilities:
- Identify patients at nutritional risk
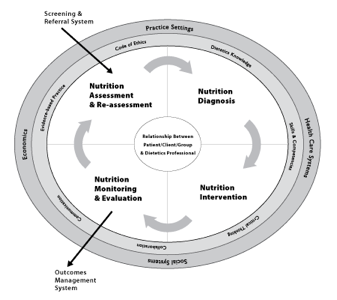
- Provide nutrition care using the Nutrition Care Process (see below)
- Determines the nutritional needs and diet restrictions for patients
- Plans therapeutic diets and implements preparation and service of meals for patients, which includes tube feedings, parenteral nutrition, and modified texture diets.
- Instructs patients and their families on healthy eating and/or special diets
- Participates in interdisciplinary discussions and meetings with other health care providers
What is the Nutrition Care Process?
The NCP is a systematic approach to providing quality nutrition-related care. It is divided into four separated, but interrelated steps: assessment, diagnosis, intervention, monitoring/evaluation.
- Nutrition Assessments – obtain, verify, and interpret data to identify nutrition-related problems, their causes, and their significance. Five main domains:
- Food/Nutrition Related History:
- Examples include:
- Allergies, intolerance, special diets
- How has the patient been eating?
- Access to food
- Anthropometric Measurements:
- Examples include:
- Height and Weight
- Calculate BMI, Ideal Body Weight, Adjusted/Feeding Body Weight
- Any weight changes?
- NOTE: use this information to calculate calorie, protein, and fluid needs
- Examples include:
- Biochemical Data, Medical Tests, and Procedures:
- Examples include:
- Lab values, test results, surgeries
- Examples include:
- Nutrition-Focused Physical Findings:
- Examples include:
- Edema, skin breakdown, hair loss
- Examples include:
- Client History:
- Examples include:
- Previous health conditions
- Examples include:
- Examples include:
- Food/Nutrition Related History:
- Nutrition Diagnosis – describe nutrition related problem using standardized language
- Commonly referred to as a PES statements
- Problem, Etiology, Signs and Symptoms
- Commonly referred to as a PES statements
- Nutrition Intervention – actions used to remedy a nutrition diagnosis/problem
- Calculate tube feeding prescriptions
- Calculate parenteral nutrition prescriptions
- Recommend nutrition supplements to meet calorie/protein needs
- Modify diet consistency or texture
- Provide nutrition education or counseling
- Nutrition Monitoring and Evaluation:
- Follow the progress of nutrition goals by monitoring weight, labs, intake and/or diet tolerance.
What patients are seen by the dietitian?
Patients of nutrition risk are seen by the RD – This can be determined by:
- Admitting diagnosis, condition, or chief complaints. Common examples include:
- Bowel Obstruction/Ileus
- Burns
- Cancer
- Celiac Disease
- Cirrhosis
- Chronic Kidney Disease
- Cystic Fibrosis
- Diabetes, new onset
- Dysphasia
- Hepatic Encephalopathy
- Malnutrition
- Pancreatitis
- Renal Failure
- Renal Transplant
- Spinal Cord or Traumatic Brain Injury
- And many more…
- NPO/Clear Liquid greater than 3 consecutive days
- New tube feeding (enteral nutrition) orders
- New parenteral nutrition orders
- Specific lab values:
- Low albumin (<2.5 mg/dL)
- Low prealbumin (<16 mg/dL)
- High blood glucose (≥200 mg/dL X 3 consecutive results)
- NICU: Phosphorus (>600 U/L)
- NICU: Bilirubin (<4.5 mg/dL)
- NICU: Alkaline phosphatase (> 2 mg/dL)
- Consults made by MD, RN, Pharm D, ancillary or patient’s family.
- May include a request for: an assessment, visit, calorie count, tube feeing, parenteral nutrition, or education.
References:
http://www.eatright.org/HealthProfessionals/content.aspx?id=7077